We just closed down our second day of clinic, and the sense of satisfaction, joy, and gratitude for our work seems genuinely shared by everyone. Even crusty old-timers have been brought occasionally to tears in the last few days. One thing was really clear after our first day on Monday: No matter what skills and special gifts those of us from the States bring to our work here, our local partners, volunteers, and support staff are what keep this program alive as it grows and serves these little communities. The staff were everywhere as we prepped the clinics this morning—moving materials and people, answering the dozens of questions we all had, and cheering us on. Julia and Tagni are two great leaders of an unforgettable and growing team. They save us hours of trial and error and mistakes by gently letting us know that there are often “different ways of doing things.” It’s hard to believe that they do this week after week with each new village team—patience, motivational words, gratitude, firm direction!
Our morning gathering in the courtyard barely over (and special Valentines candies given to everyone), we were off to our clinic assignments. One of our first patients—a little girl with her silver bracelet, bottle, and bright smile and laugh set the tone for the day’s work! Kip and the other triage staff kept busy with a steady stream of patients. General Medicine patients seemed more eager and restless than others to get this thing moving—to get in to see Carol, Lauren, and the rest of the clinic team. Several had to be reseated from time to time! I also witnessed an occasional patient circling back for a second visit to this clinic—ailments seemed to materialize and balloon the closer they got to the door! But it was probably all just my imagination….
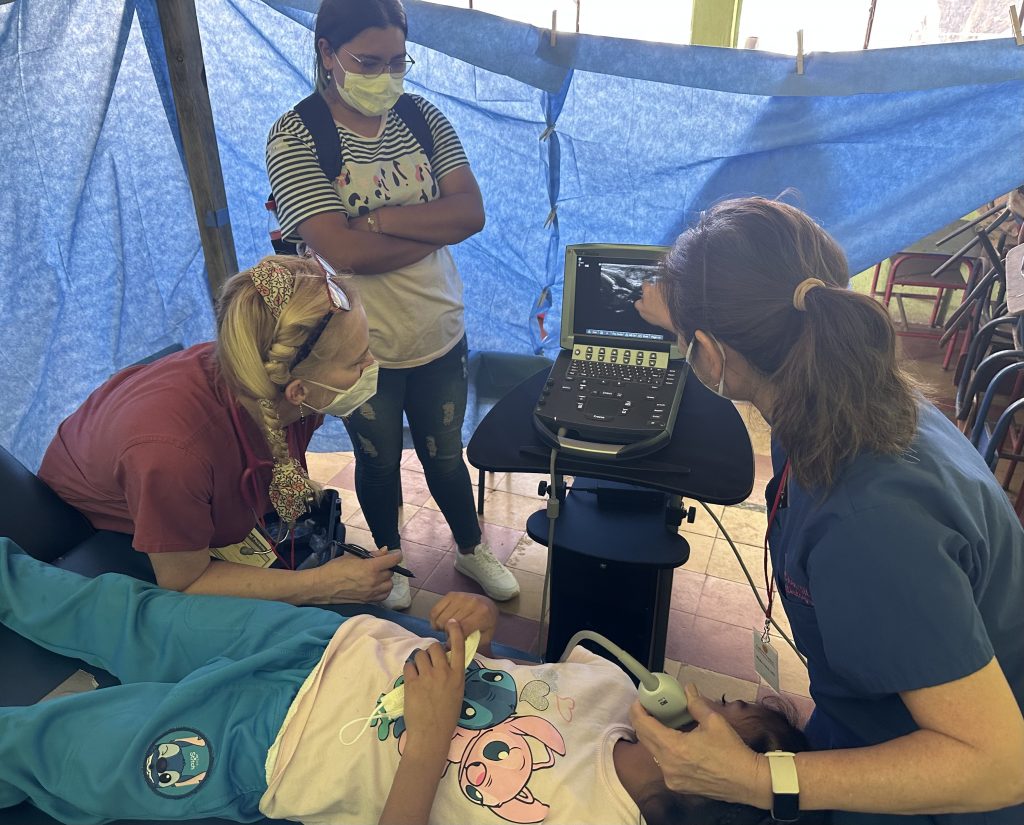
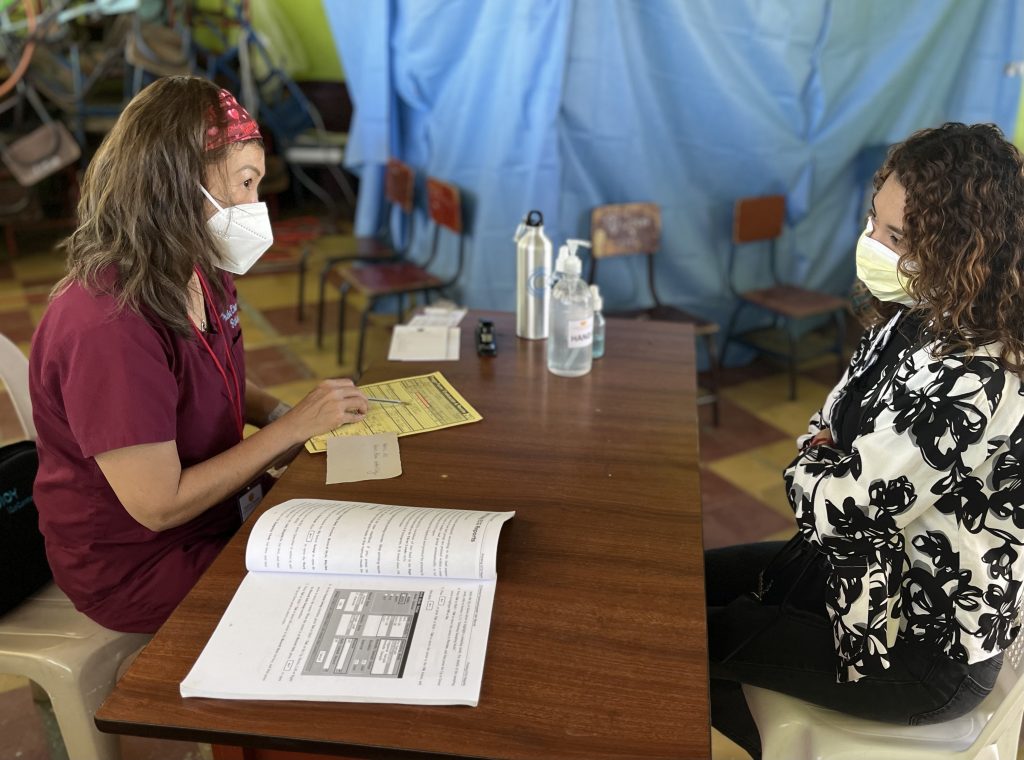
Phebe is our sole radiologist. She keeps the sonogram (and EKG) machines humming in a very in-demand clinic. She does great patient interviews from her large mahogany parquet desk with leather top and leaded crystal inkwells in the plushest room in the clinic (see picture with curtain and broken chairs and gross green walls in the background). Most of her time has been getting those very important images to her fellow providers that are often decisive in making a solid diagnosis. Yesterday she tied her all-time village mission procedures record: twenty-four sonograms and two EKGs in nine hours. Her husband Mark is over in Pediatrics. That team has been surprised by the number of hepatitis A cases presenting among young children—we seem to have dropped in on a local superspreader event, and it’s keeping everyone on their toes.
The lab is ably staffed by Joe and Brendan. This is Brendan’s first assignment with Faith in Practice, and you’ll hear from her later this week about first impressions. Lots of urine tests and diabetes finger sticks are done throughout every day. Diabetes is a serious scourge down here: A stunning 25% of the indigenous population that makes up 60% of the country’s 17 million citizens is diabetic or pre-diabetic. There are lots of complicated reasons for that, and even though the national rate for the whole country matches the rate in the US (around 10%), this illness takes a real toll on the health care system and the lives of poor families where medical attention and access to affordable medications is dismal.
Gayle Turner ran the mobility clinic back in 2020 when I served with her building and fitting wheel chairs. She was unable to make it this year, but Kathy—a fifth year physical therapy student from Antigua with loads of clinical experience and a knack for teasing out every patient’s ailments–is heading up the operation this year. This year’s clinic is limited to walkers, canes, crutches, fixing and refurbishing older equipment (my new vocation), and conducting loads of patient education that keeps her very busy. Some great referrals made today will land a couple of kids custom wheelchairs that will fit their frame and needs.
We’re able to send a lot of patients on their way satisfied with their care and their major concerns addressed. But there are many challenges, and today Mark and Michael in peds met Cristofer and his mom (he’s the young tyke in red shirt with long brown hair in our picture roll). The little guy is suffering from a myelodysplastic syndrome, which results in inadequate production of blood cells by his bone marrow. He is anemic and has a low white blood count. As a consequence, he is more susceptible to infection. The upshot is that he really needs a bone marrow transplant, and it’s a procedure that could very well mean the difference between life and death. His mom implored our clinical team to help her son out in any way we could. The sad truth is that—while we might take bone marrow transplants for various leukemias in kids for granted in the States—it is not a procedure that is presently performed in Guatemala. Fortunately, the country’s Help Me Live Foundation (AYUVI) hopes to open a pediatric bone marrow transplant center down here in the near future. In the meantime, out-of-country treatment with its prohibitive cost and the challenging logistics of travel and treatment mean that Cristofer likely won’t be able to get the care he needs to save his life. While Faith in Practice, other agencies, and the government are making palpable strides in extending care, there are limits to what can be accomplished at this time, even when we know what patients need.
Christi and Teresa in OBGYN shared a great story with us today. Yoselin, an active fifteen-year old fully engaged in school and playing futbol, came to the clinic today with a change in her health over the last year and with a sudden cessation in her periods. Mom was very concerned about this change. The providers had a suspicion that she had a condition which our village lab set-up could not test for. Our FIP team worked together to get her over to a local lab in town for some special endocrinology testing. She returned in a couple hours (!) with abnormal labs in hand, confirming the our suspicion that she had a prolactinoma, a condition that could cause changes in young womens’ menses. She was immediately referred to an endocrinology specialist in Guatemala so that she can get the appropriate imaging and medicines to help her condition. You can see her smile behind the mask and glasses as she poses with her mom and caregivers.
How amazing is that! Even in off-the-beaten path Quesada, this young girl could get a major turnaround of a lab test like that, and with a solid referral to endocrinology treatment and imaging. We can’t do everything on a one-week mission trip, but it’s so heartening that when we do see difficult cases, the ability to work through local Faith in Practice representatives can result in a patient getting the care they need—and in a country where health care resources are scarce but slowly improving, even for citizens outside of the largest cities.
We will leave you with a great picture of the dining room staff who prepared a fabulous tri-tip dinner for us tonight. What a wonderful group of people, who know what true hospitality is!
More amazing stories from the countryside of Guatemala tomorrow—stay tuned.
-Joel Zimbelman
To support this team and their commitment to our patient’s visit: