Fleeting goodbyes were extended to Dr. Ben this morning as he led us in devotions with stories and heartfelt words of motivation and blessing. He left soon after breakfast to visit additional sites in the area before heading to FIP’s base camp in Antigua.
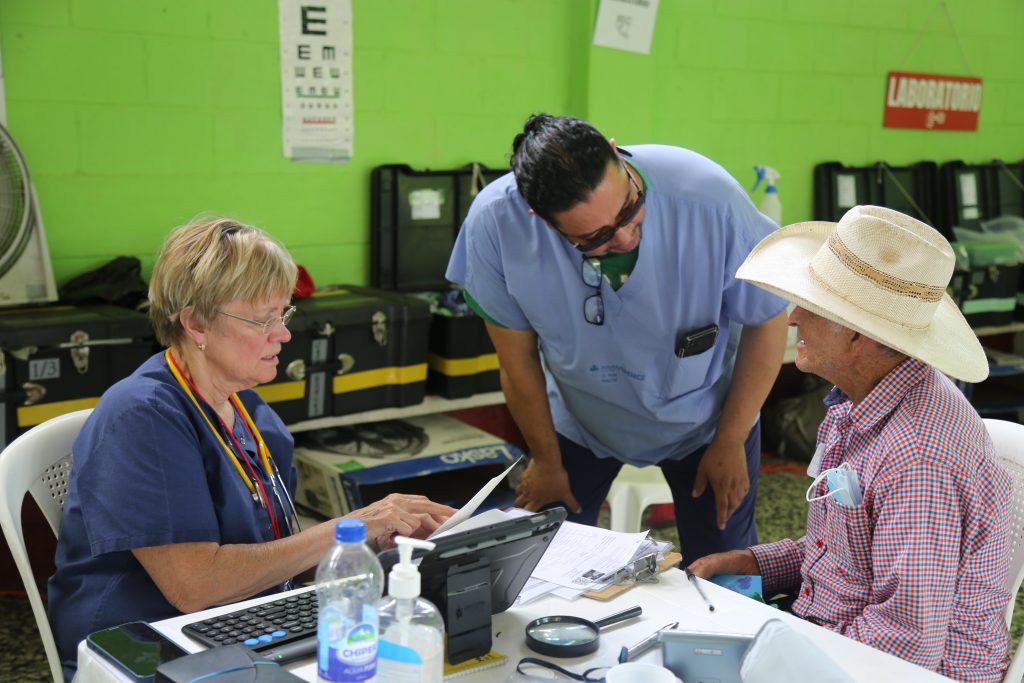
Today’s clinic offered up so many inspiring stories. But first, some insight into one of the most important roles that keeps our clinic going: The translators/interpreters that work the difficult territory of helping Spanish-speaking patients (and some staff) and English-speaking clinicians and supporting staff from the States understand each other are a resource we can’t live without. Five translators came from the States with this group, but another six from Guatemala rounded out this impressive group of language specialists. I sat down with one of Faith in Practice’s Guatemalan translators/interpreter with over ten years of translating and interpreting experience, Wolfgang Gordillo, age forty-seven and an optometrist. Wolfgang spent eleven years living in the United States and Canada before settling in Guatemala. His translation and interpreter skills, like the other five local colleagues and five from the States who joined him in this endeavor, are exceptional. FIP does not have a formal vision clinic attached to these village teams, but Wolfgang functions just great as a translator in clinical settings other than optometry. He started working with FIP teams in November, 2024. This was his third medical mission with FIP but he has lots of previous experience translating in the health care environment. His first medical mission translation gig was ten years ago when he was approached by Hearts in Motion. It’s an understatement when we say Wolfgang’s ability to interpret patient physician knowledge in a way that both our health care professionals and patient understand each other was priceless. Am I right Carol (Carol Schobert in General, and who worked with Wolfgang for three days)?
“I fell in love with taking care of the people here,” says Wolfgang. “Making a change in people’s lives; whether it’s fitting a new pair of glasses or interpreting for a medical mission or surgery mission, I could see that the volunteers at FIP feel exactly the same as I do about helping people. I feel the connection with FIP members, and I bond with them. I love working with the providers who come to Guatemala.”
Was there a moment you had at FIP, I asked, that made you choose to stay here?
“On my very first trip I felt welcomed. That made a huge difference. Other organizations felt like a paycheck. I feel loved, like there is a community that supports me. It doesn’t feel like a job. I may not know them personally, but the people I meet, I still feel connected in a way that is different from other organizations I have interpreted for. Witnessing that there are people coming down from the US who love their profession, I could see the love in the physician’s words towards the patients. I admire that.”
I asked Wolfgang: What is it like being an interpreter for FIP?
“It feels like I have a responsibility to interpret the same feeling to the patient that the physician has. Listening to every detail knowing, that the life of this person could get worse [with misunderstanding]. It’s my responsibility to make sure that the meaning of the information is right. To me it’s a huge responsibility. Also, I can feel what the person is going through in their lives and I try to communicate that. I feel good that this person is going to be ok. The experience and knowledge of these doctors is amazing. “
“When I feel that I am able to bond with the physicians that I am translating for, I sometimes get tired. But, the physicians inspire me to keep going. There’s this determination. It’s like you become a team that is dependent on each other to reach your goal.”
I asked Wolfgang how he knew what to include and what to leave out in his interpretation of the words of the patients?
“Often times a patient doesn’t understand her or his own problem, and without changing what’s going on, I try not to put words in the patients’ mouths. Regardless of what a patient is saying, I still translate it. That’s when the physician may know of a similar condition, and may ask me to ask the patient if ‘this other thing’ is also happening. If I interpreted just what I thought the issue was, the outcome of our work with the patient could be different.”
What makes a good translator and interpreter, I asked Wolfgang?
“As a translator, it’s important for there to be communication between physician and translator. As a translator, understanding involves taking oneself out of the communication process, allowing there to be nothing between physician and patient. Working with physicians as a translator has changed my life, and how I perceive. It has made me a better person, and has brought out the best in me. I finally found fulfillment in what I do and it’s deeply satisfying. It grounds me.”
My last question to Wolfgang focused on what he thought made this mission trip a success.
“I could see all of these individuals working as a team, united with the same intention. You don’t always see that. There are gaps sometimes in other groups. That’s my view from the perspective of a translator and interpreter.”
It is a blessing to know you, Wolfgang! (Wolfgang will thank the academy now) .
Another busy day in Ob/Gyn Clinic, with several additional inspirational stories. One was from a local healthcare provider who came to our clinic for her diabetes issue. It’s not a secret that Guatemala has significant women’s health gaps, especially around prenatal care and birthing. So, when we see a woman come to our clinic who is a midwife and fellow health care provider, and who is still delivering babies at the tender age of 68, it can be an emotional scene. She’s does the work that some of us do for a few days a year through our clinics, but has been doing it most days for her entire life. She is still delivering babies, and now has the prescriptions she needs to ease her challenges while doing her life’s work, tending to women and new babies of Guatemala.
In the Mobility Clinic, Dr. Filbrandt and Gayle Turner saw a young child with a severe head mass who was unable to walk. He came in for a wheelchair so his mother doesn’t have to carry him whenever he needs to move. He waited patiently for his fitting, sitting on the floor instead of a regular chair (which could not easily accommodate his frame). He really illustrates a sad fact of some of our encounters with patients: We were able to address his mobility issues and ease his challenges (and those of his family) in getting around through the provision of a wheelchair. But the challenges that he faces from his congenital cranial and face deformity are burdens we can ameliorate and that he will have to live with for the rest of his life. Still, his mother’s appreciation for the wheelchair was obvious and will make life a bit easier for this family.
Our Pediatric Clinic with Mark Ward and Joanne Reid seemed to always have long lines of patients, but young people who also seemed the most animated and engaged with their translators and clinicians. A twelve-year-old girl suffering from a very severe amalgamation of the foot came in with her parent. She was still able to go to school but has difficulty walking. It was clear that a wheelchair would help her get around, and so she headed off to Mobility for a fitting (one of our 96 wheelchairs we gave out over four days). Happily, because we have referral options and specialists attached to our Faith in Practice surgical teams, we were also able to refer her over to an orthopedic surgeon. The folks in referrals told us that for a patient like this, surgery could come as soon as four to six weeks.
Several of our mobility patients came from a village about four hours away by bus. They set out on their clinic visit about 4 a.m. By the end of the day, a truck bed filled with wheelchairs was followed by a bus filled with some children with cerebral palsy and many adults from a local nursing home with above the knee amputations. All those folks received mobility support mostly wheelchairs. The late even arrival in their village will be followed tomorrow with the chance to enjoy a more mobile and better quality of life.
Our last patient of the day was a sobering reminder of how pervasive the health care needs are of our Guatemalan patients, and the limits of our ability in many cases to help them. A forty-six year old mother of two presented with advanced cirrhosis of the liver. She had lost her entire family, and in order to cope with the trauma began to drink heavily. With no resources available to her, and no way to afford medicine, her health continued to deteriorate. Our team in General Medicine had to deliver the bad news that there was nothing we could do for her, and that she has a very short life expectancy. A referral to a GI specialist for a full work-up and some medications to ease her distress was all we could do. good news. According to general medicine, her life expectancy is short.
Another long but fulfilling day with 288 patients admitted and well over 600 discreet clinic visits. Our clinic closed a couple hours later than usual, and getting back to the hotel at 7 pm allowed for a filling dinner and some light conversation before bed, and our last day tomorrow.
Longing for espresso right now!
Eleanor, Team Blogger